Health plan managers know that a relatively small proportion of members drive a substantial portion of healthcare costs—often linked to chronic conditions and behavioral health.
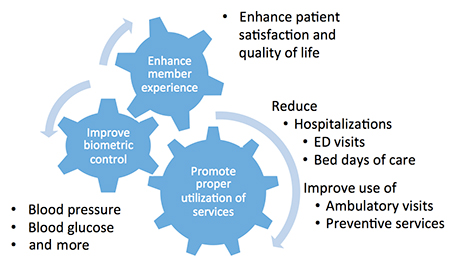
Canary Telehealth helps managed care organizations address the needs of high-risk members to enhance healthcare quality, control costs, and strengthen member satisfaction.
We remotely monitor members with uncontrolled chronic conditions and support them on their road to better self-management.
Our experienced nurses monitor target members and intervene when there is a problem. We can provide coaching and care coordination services to members or simply triage alerts for follow up by health plan case managers. Either way, these interactions provide valuable opportunities for real-time feedback and education for the member. It also shifts care to the most appropriate setting.
We take a consultative approach to remote monitoring—working alongside the health plan team to design the scope and protocols that best fit the organization and the population being managed.
Specially-trained Canary Telehealth technicians travel to member homes to provide diabetic retinopathy screening services. The images are read by a licensed eye care professional who provides an evaluation and patient instructions for follow up care. These services support health plan quality goals for diabetes care.
Canary Telehealth provides behavioral health screening through our call center. Our trained agents provide a structured, electronic diagnostic interview that screens for a wide range of adult and child disorders. The evaluation can impact multiple quality measures directly or indirectly. Behavioral health screening may also be conducted in person in conjunction with other in-home telehealth services.